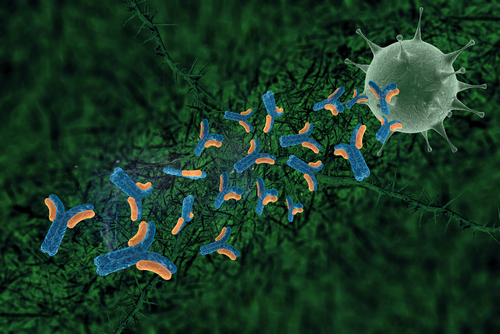
A new study led by Princeton University researchers has determined that a “triple-punch” of antibodies both prevented hepatitis C infection and wiped out the disease after it had established itself in laboratory mice Instead of administering the three antibodies conventionally, the researchers administered a genetic “instruction set” that, once entering a cell, developed into antibodies that target portions of the virus that do not mutate. A Princeton release reports that these mice treated with the antibody genetic code resisted becoming infected with hepatitis C when they were exposed to the virus.
A new study led by Princeton University researchers has determined that a “triple-punch” of antibodies both prevented hepatitis C infection and wiped out the disease after it had established itself in laboratory mice Instead of administering the three antibodies conventionally, the researchers administered a genetic “instruction set” that, once entering a cell, developed into antibodies that target portions of the virus that do not mutate. A Princeton release reports that these mice treated with the antibody genetic code resisted becoming infected with hepatitis C when they were exposed to the virus.
According to a research report published in the Sept. 17 issue of the journal Science Translational Medicine, the scientists also gave the antibodies to already infected mice and found that, in many cases, the infection disappeared to levels below detection.
The research article, entitled “Broadly neutralizing antibodies abrogate established hepatitis C virus infection” (Sci Transl Med 17 September 2014: Vol. 6, Issue 254, p. 254ra129 DOI: 10.1126/scitranslmed.3009512 ) is coauthored by Ype P. de Jong of the Center for the Study of Hepatitis C, Division of Gastroenterology and Hepatology at Weill Cornell Medical College, New York; Marcus Dorner, Michiel C. Mommersteeg, Jing W. Xiao, Kevin Vega, Sherif Gerges, Rachael N. Labitt, Bridget M. Donovan, and Charles M. Rice, of the Center for the Study of Hepatitis C, Laboratory of Virology and Infectious Disease, The Rockefeller University, New York; Alejandro B. Balazs and Dennis R. Burton of the Ragon Institute of MGH, MIT and Harvard, Cambridge, Massachusetts; Mansun Law, Justin B. Robbins and Erick Giang of the Department of Immunology and Microbial Science, The Scripps Research Institute, La Jolla, California; Alexander Ploss and Benjamin Y. Winer of the Department of Molecular Biology, Princeton University, Princeton, NJ; Anuradha Krishnan and Michael R. Charlton of the Division of Gastroenterology and Hepatology, Mayo Clinic College of Medicine, Rochester, Minnesota; Luis Chiriboga of the Department of Pathology, New York University Medical Center, New York; and David Baltimore of the Division of Biology, California Institute of Technology, Pasadena, California.
The researchers note that in most exposed individuals, hepatitis C virus (HCV) establishes a chronic infection, and this long-term infection in turn contributes to development of liver diseases such as cirrhosis and hepatocellular carcinoma. They observe that the role of antibodies directed against HCV in disease progression is poorly understood. Neutralizing antibodies (nAbs) can prevent HCV infection in vitro and in animal models, but the effects of nAbs on an established HCV infection are unclear. In this study, they demonstrate that three broadly nAbs—AR3A, AR3B, and AR4A—delivered with adeno-associated viral vectors can confer protection against viral challenge in humanized mice. Furthermore, they provide evidence that nAbs can abrogate an ongoing HCV infection in primary hepatocyte cultures and in a human liver chimeric mouse model. They say tese results showcase a therapeutic approach to interfere with HCV infection by exploiting a previously unappreciated need for HCV to continuously infect new hepatocytes to sustain a chronic infection.
The Princeton release notes that Hepatitis C affects roughly 170 million people worldwide and causes chronic liver damage and cancer. The virus is most typically transmitted to humans via contact with contaminated blood during intravenous drug use or medical procedures, and attempts to develop a hepatitis C vaccine have been hampered by the virus’s ability to mutate into numerous subtypes. This genetic diversity is a barrier to developing traditional vaccines, which work by eliciting an immune response against a specific protein or other feature on the surface of the viral particle. These protein targets frequently change when the virus mutates.
 To circumvent this problem, the researchers selected antibodies known to target parts of the virus that tend not to change during mutation, explains the paper’s lead author Alexander Ploss, an assistant professor in Princeton’s Department of Molecular Biology. Such antibodies are called “broadly neutralizing” because they deactivate a variety of genetic subtypes. The ones used in the study were discovered by co-author Mansun Law and his
To circumvent this problem, the researchers selected antibodies known to target parts of the virus that tend not to change during mutation, explains the paper’s lead author Alexander Ploss, an assistant professor in Princeton’s Department of Molecular Biology. Such antibodies are called “broadly neutralizing” because they deactivate a variety of genetic subtypes. The ones used in the study were discovered by co-author Mansun Law and his  team at the Scripps Research Institute’s Law Lab in La Jolla, California.
team at the Scripps Research Institute’s Law Lab in La Jolla, California.
As Dr. Ploss notes, rather than injecting the actual antibodies which can be degraded before reaching their targets the researchers injected the genetic instructions for making the three antibodies. These instructions consist of the antibodies’ genetic codes, or DNA, each linked to the DNA for a benign virus called adeno-associated virus (AAV)These instructions consist of the antibodies’ genetic codes, or DNA, each linked to the DNA for a benign virus called adeno-associated virus (AAV). This virus acts as a ferry that brings the antibody genes into cells, a delivery technique pioneered by study co- author David Baltimore and colleagues at the California Institute of Technology’s Baltimore Lab which is involved in two major research thrusts: basic investigation of the development and functioning of the mammalian immune system; and Engineering Immunity: translational studies using viral vectors to carry new genes into immune cells to increase the range of pathogens effectively fought by the immune system and to make the immune system resist cancer growth more effectively. The Baltimore Lab’s basic studies have two directions: to understand the remarkable range of activity of the NF-kB transcription factor and to understand the normal and pathologic functions of microRNAS. NF-kB activates perhaps 1000 genes in response to a wide range of stimuli. It has different physiologic roles in different cells. How one factor can be so varied in its activity is the puzzle that has interested researcehers for many years and that the lab team studies at many different levels.
author David Baltimore and colleagues at the California Institute of Technology’s Baltimore Lab which is involved in two major research thrusts: basic investigation of the development and functioning of the mammalian immune system; and Engineering Immunity: translational studies using viral vectors to carry new genes into immune cells to increase the range of pathogens effectively fought by the immune system and to make the immune system resist cancer growth more effectively. The Baltimore Lab’s basic studies have two directions: to understand the remarkable range of activity of the NF-kB transcription factor and to understand the normal and pathologic functions of microRNAS. NF-kB activates perhaps 1000 genes in response to a wide range of stimuli. It has different physiologic roles in different cells. How one factor can be so varied in its activity is the puzzle that has interested researcehers for many years and that the lab team studies at many different levels.
Research in Dr. Ploss’s lab at Princeton focuses on immune responses and pathogenesis to human pathogens infecting the liver, including hepatitis B (HBV) and C viruses (HCV), yellow fever and Dengue viruses and plasmodial parasites. The Ploss lab research group combines tissue engineering, molecular virology/pathogenesis, and animal construction, to create and apply innovative technologies for the study and intervention of human hepatotropic infections. Dr. Ploss’s research focuses on immune responses and pathogenesis to human infectious diseases, including hepatitis C virus, yellow fever virus, and malaria. His group combines tissue engineering, molecular virology/pathogenesis, and animal construction, to create and apply innovative technologies including humanized mouse models for the study and intervention of human hepatotropic infections. In recognition of his work he received a Kimberly Lawrence Cancer Research Discovery Fund Award, the Astellas Young Investigator Award of the Infectious Diseases Society of America and the Liver Scholar Award from the American Liver Foundation.
Once inside the cells, the genetic codes were translated by the cell’s machinery into hepatitis C antibodies, which were excreted into the bloodstream where they attached to the proteins on the viral surface to inactivate them.
The investigators found that mice injected with the AAV-antibody particles went on to develop high and sustained levels of the antibodies against the virus in their blood, and these antibodies protected them from becoming infected when they were later exposed to the virus. “The treatment is a single intramuscular injection that results in high quantities of antibodies in circulation for several months,” Dr. Ploss says.
The researchers also tried the AAV-antibody treatment on mice that already had a hepatitis C infection. “We weren’t sure we would see any results because the antibody can only neutralize viruses that are outside of cells, whereas viral replication is taking place inside the cell, but we decided to try it,” Dr. Ploss explains. “The surprising thing was that within several weeks we saw a decrease in the level of virus in the blood, and in many of the mice, their virus level went below the limit of detection.”
Dr. Ploss cautions that the studies in mice would have to be replicated in human clinical trials, a step that could be a long way off. But new approaches for preventing hepatitis C are needed given how widespread the virus is in many parts of the world. Roughly eight out of every 10 people with the virus develop a chronic infection that leads to progressive liver disease and scarring. Yet most infected individuals do not display symptoms for a decade or more. A drug that came on the market in 2013 can cure the disease, but the high cost may prevent or delay widespread use, especially in developing countries.
 Dr. Michael Houghton, a faculty member at the University of Alberta who, with colleagues, discovered the hepatitis C virus in 1989, said that the research by Dr. Ploss and his co-authors shows potential for developing an effective and affordable treatment for the virus.
Dr. Michael Houghton, a faculty member at the University of Alberta who, with colleagues, discovered the hepatitis C virus in 1989, said that the research by Dr. Ploss and his co-authors shows potential for developing an effective and affordable treatment for the virus.
“This work is very important since it shows that a combination of neutralizing antibodies against the hepatitis C virus can restrict viral spread in the liver thereby ameliorating, and possibly curing, chronic infection,” says Dr. Houghton, who was not involved in the current study but is familiar with it, in the Princeton release. “The current work opens up the possibility of treating more patients in a less expensive way and also gives the patient and clinician more treatment options for a disease that affects 170 million people worldwide.”
The study also provides evidence for the use of antibody-based strategies to prevent hepatitis C infection, Dr. Ploss observes. “Much of the current research on vaccines is focused on stimulating the part of the immune system that involves T cells [which are white blood cells with a central role in the body’s response to pathogens],” Ploss said, “but our study suggests that broadly neutralizing antibodies could be an important component of an effective hepatitis C vaccine.”
The ability of the antibody to remove an existing infection may shed light on how the virus maintains a chronic infection in humans, Ploss said. “Our results seem to suggest that to sustain a persistent infection, the virus must continually infect new cells rather than relying on an existing set of infected cells,” he continues. “When we inject antibodies that destroy the viral particles, we may be breaking this chain of infection. This suggests that long-term treatment with broadly neutralizing antibodies could be effective at treating existing infection.”
 Because hepatitis C virus is a human infection that does not naturally occur in other animals, the researchers used two strains of mice with human-like livers that were developed by D. Ploss and colleagues at Rockefeller University in New York City, including the study’s first author, Ype de Jong, now an assistant professor of medicine at the Weill Cornell Medical College. In one strain, the mouse-liver cells express human molecules required for viral uptake, while in the strain developed with Dr. de Jong, the mice livers contain human cells.
Because hepatitis C virus is a human infection that does not naturally occur in other animals, the researchers used two strains of mice with human-like livers that were developed by D. Ploss and colleagues at Rockefeller University in New York City, including the study’s first author, Ype de Jong, now an assistant professor of medicine at the Weill Cornell Medical College. In one strain, the mouse-liver cells express human molecules required for viral uptake, while in the strain developed with Dr. de Jong, the mice livers contain human cells.
In addition to the authors mentioned above, the study included graduate student Benjamin Winer and research specialist Sherif Gerges of Princeton University; Marcus Dorner, Michiel Mommersteeg, Jing Xiao, Kevin Vega, Rachael Labitt, Bridget Donovan and Charles Rice of Rockefeller University; Alejandro Balazs and Dennis Burton of the Ragon Institute of MGH, MIT and Harvard; Erick Giang, Justin Robbins of the Scripps Research Institute; Anuradha Krishnan and Michael Charlton of the Mayo Clinic College of Medicine, and Luis Chiriboga of New York University Medical Center.
Support for the work came from grants from the National Institute of Diabetes and Digestive and Kidney Diseases; the National Institute for Allergy and Infectious Disease (grant nos. K08DK090576, R01AI072613, R01AI099284, R01 AI10730101, and R01AI071084); the National Cancer Institute (grant no. R01CA057973); the Bill and Melinda Gates Foundation; the Starr Foundation; the Greenberg Medical Research Institute; the Richard Salomon Family Foundation; the Ronald A. Shellow, M.D. Memorial Fund; the MGM Mirage Voice Foundation; Gregory F. Lloyd Memorial contributions; and anonymous donors.
Sources:
Princeton University
Science Translational Medicine
California Institute of Technology
The Scripps Research Institute